Debunking Common Myths About Low Back Pain
- Jeffrey Ragosta
- Feb 11
- 7 min read
Updated: Feb 12
Debunking common myths about low back pain
There is absolutely no doubt that low back pain is a huge issue. Latest evidence shows that in 2020 alone, there were 619 MILLION people globally with low back pain. Due to the aging population and more sedentary workplace responsibilities, that number is projected to rise to 843 MILLION by 2050 (1) .
Let’s now talk dollars and cents. Research conducted by Kirsch et. al in April 2024 found that people who utilized the US healthcare system a lot, (surgeries, emergency visits, prescriptions, etc.) spent an average of $31,459 dollars in low back pain related costs over the first 5 years since being officially diagnosed (2) . So many people have it, so many people spend so much money trying to get rid of it!
That being said, having sharp pain which hinders and or stops you from doing the things you need to do/love to do is NOT OKAY. There’s something you can do about it! Don’t let it catch up to you and before you know it, you’re paying for another MRI, going to another specialist, getting another surgery. It can be a vicious cycle, address it NOW!
“Once I have low back pain, I’ll have it forever”
I’ve heard this one all too much. Countless times I have encountered people who are at least 70 years old and when I ask them how long they have been dealing with low back pain, their response is something like… “since I was 17”, “football injury in college”, “oh for as long as I can remember”. If we deal with pain and recurring injuries for years upon years, there’s actually changes that happen in your central nervous system. It can lower your nervous system's sensitivity to pain thresholds causing abnormal responses to routine stimuli, negatively affect your ability to emotionally process pain, increase your risk of having depression, and overall decrease your ability quality of life (3) .
Do not succumb to your pain and make it part of your identity. You CAN do something about it. Rather than just treating the symptoms and spending thousands of unnecessary dollars on things that hardly provide relief, let’s find the ROOT CAUSE of your pain together! I want to see you out doing what you love, pain free.
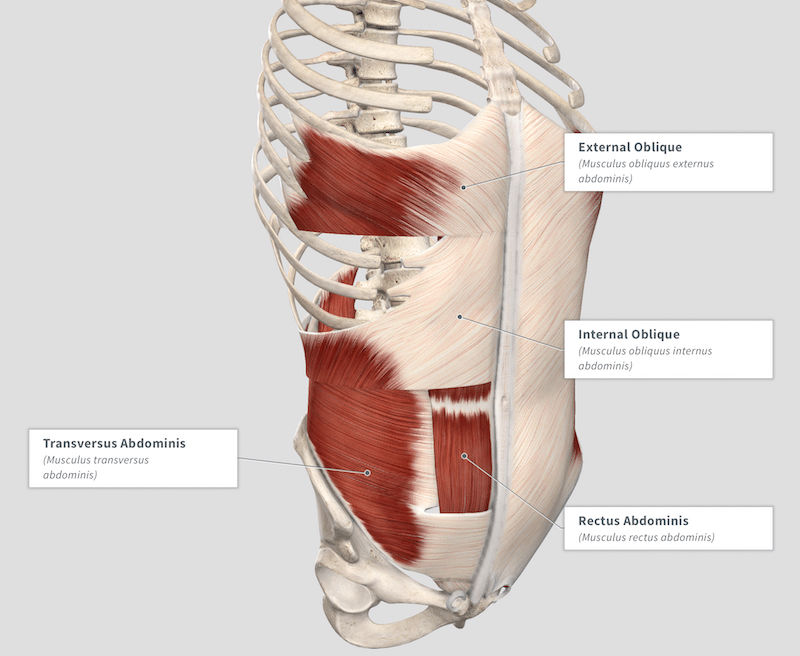
Contrary to popular belief, you CAN absolutely manage your chronic low back pain. Decreasing overall intensity of pain, increasing time between flare-ups, and improving your activity tolerance. However, it’s all about finding the root cause! Addressing specific abhorrent movement patterns developed over time, finding muscle strength/coordination imbalances, and ensuring muscle flexibility is sufficient enough to function in optimal ways.
“If I lose weight, my pain will go away”
I’ve heard this one quite a bit recently. If you are “overweight”, chances are dietary changes and an exercise program will greatly help you. However, speaking with a licensed healthcare professional before engaging in any sort of new health related behavior is highly recommended. As we all know, being overweight and or obese can cause a plethora of health issues. High blood pressure, increased risk of diabetes and heart disease are just the tip of the iceberg.
One of these potential effects of being overweight is excessive strain on your joints. Having excessive adipose tissue, especially over a long period of time can force your soft tissues and joints to work harder than usual. This can create a recipe for disaster, opening the door for chronic pain. Obese individuals tend to report higher levels of pain in many weight bearing joints like the hips, knees, and hands (4) .
Being of a healthy weight and body composition has innumerable health benefits. Not just your physical health either…regular exercise can boost energy levels, improve cognitive function, and improve sleep quality. BUT…if you do not address the ROOT CAUSE of your symptoms, you will not see significant lasting effects. You can be as healthy as you can be, if you still lift with improper technique and have poor posture all day at work, you will not get fully better.
Short answer, losing weight if you are obese, will definitely help your pain but it will NOT cure it. It’s only a band aid.
“Low back surgery is bad, I’ll never be the same after that”
Piggybacking off the last point, I think again this myth directly relates to individuals not addressing the root cause of the symptoms. Research in 2023 looked at over 11,000 people who underwent surgical intervention for lumbar stenosis. They found that over 70% of their group were deemed good outcomes. Strongest predictors of negative outcomes or “failures” after surgery were age > 70, long duration of symptoms, and previous lumbar surgery (5) .
There’s definitely a time and place for surgery. Sometimes no matter how strong and stable the surrounding structures are, there are structural abnormalities that can really only be fully corrected with surgical intervention. If you can avoid surgery, wonderful, it should be the last resort if conservative treatments fail. BUT, if multiple providers tell you surgery may be a good idea, do not fear the outcome. Put in the work, do the rehab exercises afterwards, odds are in your favor that you’ll have a positive outcome.
Here’s another hopeful graphic:

*from 2020 research looking at satisfaction of lumbar surgery within 1 year of surgery and 5 years afterwards. You can see the majority of the graphs are successes! (6) .
“My back is horrible, MRI said I have degenerative changes and some herniated discs”
Two things in research that are very important to consider when looking at the accuracy of a diagnostic test are sensitivity and specificity. To quickly summarize, if a test has a high sensitivity, the test is very good at correctly identifying people with the tested condition. Highly sensitive tests have a low chance of false negatives. If a test has high specificity, the test is very good at correctly identifying people without the tested condition.
So, if a highly sensitive test is NEGATIVE, there’s a good chance you do not have the condition being tested for.
On the other hand, if a highly specific test is POSITIVE, there’s a good chance you do have the condition being tested for.

picture source: https://emcrit.org/pulmcrit/mythbusting-sensitivity-specificity/
The only reason why I even mention the statistical analysis of things is because lumbar MRI’s are very sensitive, but not very specific. Meaning, there’s a greater likelihood that a lumbar MRI would identify false positives such as disc herniations and degenerative changes (7) .
Research shows sensitivity numbers for lumbar disc herniations from 89-100%
Specificity for lumbar disc herniations have been found to be as low as 43-97% (8) .
The big takeaway here is that don’t think of a lumbar MRI as an “end all be all” type diagnostic test. Yes, it’s wonderful to actually see the inside of your spine so providers can get a better understanding of what’s going on. However, DO NOT be alarmed and think it’s the worst thing in the world if you see “degenerative changes” and or “mild disc herniations” on your report. There’s a good chance that if we took lumbar MRI’s on healthy individuals without pain, there will be some who will show degenerative changes and disc herniations.
“I’ve got a bad back, I can’t exercise”
Rest is good, for sure. Especially after an acute injury or a flare up of some old pain, taking it easy for 24-48 hours after the injury is a great idea. However, too much rest can be very harmful. Consistent findings across the medical literature indicate that advice to continue with ordinary activities and gradually return to pre-injury levels of activity can expedite recovery time, decrease risk of recurrent problem, and decrease social/emotional impact of pain and disability (9) .
Not to mention, staying in bed and resting for too long can stiffen muscles, decrease synovial fluid distribution in your joints (resulting in stiff, painful joints), and can promote unwanted absorbent movement patterns, especially if you’re sitting in poor postures.
That’s why, after the initial pain starts to subside, a gentle and appropriately graded exercise program will get you back to doing what you love sooner and lessen the chance of the pain coming back in the future. We will pinpoint the root cause of your pain and give you a specific program designed to give you long term positive effects.
References
GBD 2021 Low Back Pain Collaborators. “Global, Regional, and National Burden of Low Back Pain, 1990-2020, Its Attributable Risk Factors, and Projections to 2050: A Systematic Analysis of the Global Burden of Disease Study 2021.” The Lancet. Rheumatology, vol. 5, no. 6, June 2023, pp. e316–29. PubMed, https://doi.org/10.1016/S2665-9913(23)00098-X.
Kirsch, Elayna P., et al. “Healthcare Resource Utilization for Chronic Low Back Pain among High-Utilizers.” The Spine Journal, vol. 24, no. 4, Apr. 2024, pp. 601–16. ScienceDirect, https://doi.org/10.1016/j.spinee.2023.11.017.
Yang, Seoyon, and Min Cheol Chang. “Chronic Pain: Structural and Functional Changes in Brain Structures and Associated Negative Affective States.” International Journal of Molecular Sciences, vol. 20, no. 13, June 2019, p. 3130. PubMed Central, https://doi.org/10.3390/ijms20133130.
Gløersen, M., et al. “Associations between Overweight/Obesity and Joint Pain in Persons with Hand Osteoarthritis: Results from the nor-Hand Study.” Osteoarthritis and Cartilage, vol. 28, Apr. 2020, p. S137. DOI.org (Crossref), https://doi.org/10.1016/j.joca.2020.02.227.
Alhaug, Ole Kristian, et al. “Predictors for Failure after Surgery for Lumbar Spinal Stenosis: A Prospective Observational Study.” The Spine Journal, vol. 23, no. 2, Feb. 2023, pp. 261–70. DOI.org (Crossref), https://doi.org/10.1016/j.spinee.2022.10.010.
Tuomainen, I., et al. “Unfolding the Outcomes of Surgical Treatment of Lumbar Spinal Stenosis—a Prospective 5- and 10-Year Follow-up Study.” European Spine Journal, vol. 29, no. 9, Sept. 2020, pp. 2231–42. link.springer.com, https://doi.org/10.1007/s00586-020-06424-5.
Yong, Xian Zhang Eric, and Tom Sutherland. “Making Sense of MRI of the Lumbar Spine.” Australian Family Physician, vol. 41, no. 11, Nov. 2012, pp. 887–90.
Jarvik, Jeffrey G., et al. “Three-Year Incidence of Low Back Pain in an Initially Asymptomatic Cohort: Clinical and Imaging Risk Factors.” Spine, vol. 30, no. 13, July 2005, pp. 1541–48; discussion 1549. PubMed, https://doi.org/10.1097/01.brs.0000167536.60002.87.
Waddell, G., et al. “Systematic Reviews of Bed Rest and Advice to Stay Active for Acute Low Back Pain.” The British Journal of General Practice, vol. 47, no. 423, Oct. 1997, pp. 647–52. PubMed Central, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1410119/.



Comments